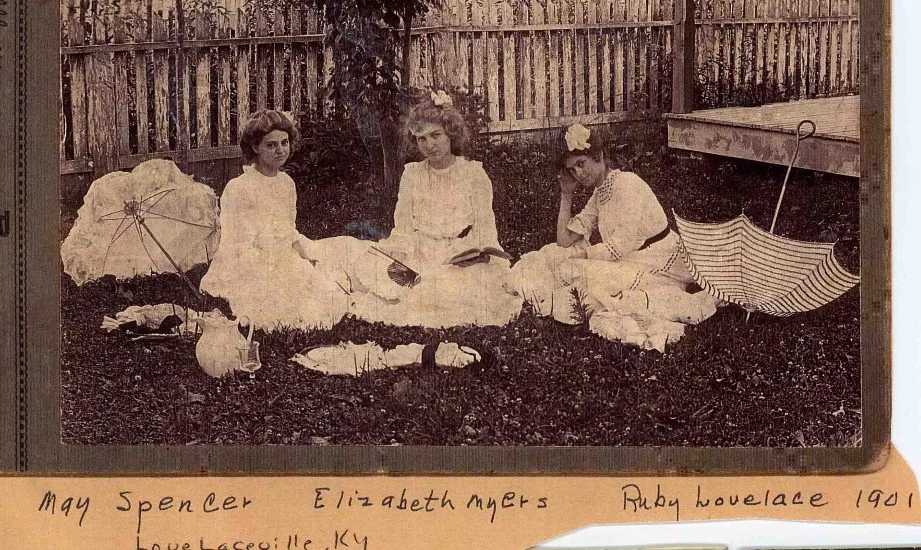
Lucia then
Amelia then
When I was pregnant with my twins in 2009, my Type-A personality kicked in to overdrive and I became obsessed with preparing our lives for these two little creatures. I carefully researched products, joined my local twins club for advice and support, and took a twins preparation class (“Twiniversity 101”). Being the control freak I am, I chose to deliver at the hospital with the best NICU in New York City and I switched to one of the best high-risk obstetrics practices, whereI insisted on weekly monitoring for any signs of preterm labor. I know that twins often come early and I was prepared for that possibility. Or so I thought. When my water broke suddenly at 30 weeks and my doctor informed me that the babies would be arriving imminently, I could not have felt less prepared. I wasn’t ready. I sobbed over and over that THEY weren’t ready. It wasn’t time yet. I held on for five days and then, at barely 31 weeks, my Baby A, Lucia, came roaring out with a bang, almost in the elevator. Baby B, Amelia, was distinctively less gung-ho to leave the warm, cozy womb (understandably) and she ambled out 5 hours and 12 minutes later. (Seventeen months later, this pretty much still says it all about their personalities.) At birth, Lucia weighed 2 pounds 15 ounces and Amelia weighed 3 pounds 6 ounces. Both girls were so tiny and so fragile, barely moving, and all I could think was that they shouldn’t be here yet. So began our NICU journey, which continued for the longest six weeks and two days of my life.
I am part of a wonderful community of mothers of twins (and a few fathers) here in NYC. Most of us had a long, difficult road to parenthood, and far too many of us endured days, weeks, and even months with our newborns confined to plastic incubators in hospital NICUs instead of at home with us. I naturally turned to my fellow twin moms when compiling a list of advice a few months ago for a friend of a friend’s sister (you know how that goes) who had just had preemie twins. The list that follows reflects my own experience in the NICU, along with the input of many of my fellow warrior moms. (We are indeed a special breed of mothers. The first few months of life with preemie twins feels like intense training to a be some sort of ninja warrior mom. Or a special edition of “Survivor: Twins.”)
1. You may not fall instantly in love with your baby/ies. You always imagine that just after your baby is born, the doctor will lay the baby on your chest, you’ll gaze into each others’ eyes, and you’ll immediately be overcome with a powerful love for your new baby. This is not what happens when you give birth to premature or sick babies. The second that baby emerges, there is an army of doctors, nurses, interns, residents, neonatalogists, and other assorted random people in the room who will whisk your baby/ies away before you even have a chance to realize that you’ve just given birth. I didn’t even get a glimpse of my babies until many hours after they were born, and that was only for a couple of minutes. I was not able to hold Lucia until about a week after she was born. Amelia was less stable, so it was even longer before I was permitted to touch her, and I only held her a handful of times during her first month of life. Our emotions were impossibly complicated during those early weeks: We didn’t feel “love” for our babies so much as an overwhelming sense of responsibility; we were in a state of limbo in which our children were “here” but they weren’t really here yet; we had children but we didn’t feel like we were parents yet. If you had asked me during that time if I had any children, I would have hesitated before answering. It wasn’t until Lucia and Amelia were about 8 weeks old that I was able to say “I love you” to them and that I really felt as though I loved them. But once I started, I couldn’t stop! (I’m pretty sure that by the time they are 13 years old and I am still telling them I love them 56 times a day, they are going to be really annoyed.)
2. Pick a primary nurse to care for your baby/ies. After a few days of getting to know the staff, it’s a good idea to pick a couple of nurses who you particularly like and ask the charge nurse that these nurses be assigned to your baby/ies as much as possible. Each nurse has a different style and different ideas about the best way to care for babies. The conflicting information from all of the different nurses about every little thing from the best swaddling technique to proper pacifier size will drive you nuts. Having one or two nurses you know and trust will help your own peace of mind and ensure continuity of care for your baby/ies.
3. You do not have to spend every waking moment in the NICU. The NICU nurses are the best babysitters you will ever have. Take advantage of this time to go out to dinner, see a movie, or get a massage. This is easier said than done when you have a baby or two in the hospital, but it is important to take a little time for yourself while you can. (Full disclosure: I was never able to put this into practice. I spent every waking minute at the hospital, with the exception of New Year’s Eve when I found myself drunkenly sobbing while pumping and dumping in the bathroom stall of crowded bar. But you should learn from me and not do that.)
4. Having your twins come home together is overrated. Twins rarely are released from the hospital on the same day. Baby A usually is a little stronger and is ready to go home before Baby B, who has a few more issues to overcome. (This is a fact and I asked around at the hospital repeatedly but could not for the life of me come up with a medical explanation as to why this is the case.) In our case, Lucia came home over a week before Amelia. When we were told they would not be ready on the same day, I went into a panic at how we would manage to have one baby in the hospital and one at home. It seemed too overwhelming. But after the fact, I think it worked out for the best because we had a little time to figure out how to incorporate one baby into our home before introducing the second one... at which point the complete chaos began and there was no turning back.
5. You absolutely, no question, without a doubt can breastfeed your baby/ies and you can breastfeed exclusively. Breastfeeding premature twins is the hardest thing I have ever done in my life. It is also the best, most rewarding thing I have ever done in my life. I have heard a lot of women say, “My babies were in the NICU so I couldn’t breastfeed,” but having babies in the NICU does not preclude breastfeeding. Right after my girls were born, I requested that a breast pump be brought to my room and that a lactation consultant stop by to help. From day one, I pumped for 20 minutes every 2-3 hours. At first I used the lactation room in the NICU, then I requested the hospital provide me with a pump to keep in my little corner of the NICU. I rented a hospital-grade pump for my home. (The Medela Classic is the best, most powerful pump, followed closely by the Medela Symphony.) I bought a Medela Pump-in-Style totebag and a handpump for my purse to cover any rare moments when I was not at the hospital or at home. I pumped the bejeezus out of my poor, sore, screaming breasts day and night. I drank gallons of water every day. I ate cheeseburgers as much as possible. I produced enough milk for Lucia, Amelia, and a small country. I kept the NICU freezer stocked with my breastmilk at all times and I made sure that every nurse who got anywhere near my babies knew that they were to get only breastmilk in their feeding tubes. I ended up breastfeeding for nine months, exclusively for six. (Once the feeding tubes were out towards the end of the NICU stay, making the transition to nursing was a monstrous challenge. So much so that it is a topic all its own, one for another day.)
Lucia now
Amelia now
6. Get to know the medical professionals caring for your children and make a point of meeting with them every single day to ask questions, no matter how minor. Introduce yourself to the pediatrician/s assigned to your baby. Introduce yourself to the charge nurse. Get to know the nurses in your area of the NICU. If your NICU is in a teaching hospital, find out what time rounds are and stand next to your baby/ies each day as the interns present to the attending. If you are in a large and crowded NICU, this may be the only way you’ll learn exactly what is going on with your babies and follow their progress. Be ready with questions. Jump in with questions during the presentation if there are words or concepts that you don’t understand. Each morning when you arrive, ask a nurse to notify the pediatrician that you would like to see him/her at some point during the day. If you are not proactive, you may discover that the hospital staff are too busy and overwhelmed with their own work to keep you in the loop.
7. Ask for a tour of the NICU, any materials on premature babies, and to explain all of the instrumentation, monitors and other tubes wires and blinking lights attached to your baby/ies. Days went by before anyone felt the need to explain the 83 different tubes and wires coming out of my babies’ noses and mouths and attached to their little arms, stomachs and feet. Lights would blink and alarms would sound and we had no idea what was going on. About a week after my babies were born, one of the staff members offered to take me on a tour of the NICU. As part of my exit package when we were discharged from the NICU, I was given all sorts of brochures on having premature babies that explained what to expect in the NICU, the terms most commonly used (“ brady,” “apnea,” “desat”... what???), and what all of the different monitors measure and what the numbers all mean. Let me tell you, this would have been helpful BEFORE I was walking out the door of the NICU. I was really irritated.
8. Nurses are the best teachers of newborn care. The one advantage of having babies in the NICU was that by the time they came home from the hospital, we were pros at newborn care and felt totally comfortable taking care of our babies. The NICU nurses have fabulous tips for how to best swaddle, hold, position, comfort, change, burp, bathe, and feed your baby/ies. Learn from them.
9. Do kangaroo care. “Kangaroo care” is when you strip your baby down to its diaper and hold her against your bare chest while resting in a chair or rocker for a couple ofhours or so. Studies have shown that kangaroo care can improve outcomes for premature and sick babies and can shorten the amount of time spent in the NICU. Kangaroo care is trickier than it seems because a nurse has to help you finagle all of the tubes and wires to transfer the baby from the isolette to your chest and then back into the isolette a couple of hours later, and while many nurses will be great advocates for you and happily assist, some nurses just can’t be bothered. I had many more nurses in the “can’t be bothered” camp and I wish I had pushed for more kangaroo care time with my babies.
10. This will all be a distant memory before you know it. I promise.
Allison Harris is a Lawyer Mom with Twins ("LMWT") in New York City and spends an inordinate amount of time corresponding with other twin moms. She recently managed to find the elusive job that offers actual work-life balance, enabling her to put her expensive law school education to good use while also enjoying plenty of time at home with The Ladies, weekend yoga classes, and regular dinners out with other LMWT.
This post originally appeared on Salt & Nectar.